In a sub-journal of Science, the "morphing techniques" and recurrence mysteries of glioblastoma have been unveiled by Chen Liang, Liu Baohui, and Gu Ying.
Glioblastoma (GBM) is recognized as a "terminal disease" among brain tumors. The reasons for its dreadfulness are multifaceted. Despite the concurrent use of the "three major treatments"—surgery, radiotherapy, and chemotherapy—the median survival time for patients remains a mere 15 months. This tumor can be likened to an unending "battle of attack and defense." Even when the visible tumor is seemingly "eradicated," residual cells may lie dormant, awaiting an opportunity to re-emerge and trigger recurrence.
The two major characteristics of GBM—heterogeneity and invasiveness are crucial.
Tumor cells with "thousands of faces for thousands of people"
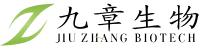
The heterogeneity of GBM is characterized by the diversity of its tumor cells, which are not uniform. Instead, there are four main states: NPC-like (neural precursor-like), OPC-like (oligodendrocyte precursor-like), AC-like (astrocyte-like), and MES-like (mesenchymal-like). These states can interconvert, akin to Transformers, adapting to environmental changes at any time. Moreover, this "transformation technique" enables tumor cells to rapidly develop drug resistance under treatment pressure and evade elimination.
The Dissemination Technique of the "Lurkers"
Another major challenge is the invasiveness of GBM. Tumor cells quietly infiltrate normal brain tissue, becoming "lurkers" that lie in wait in areas distant from the tumor core. Upon treatment cessation, these hidden cells reactivate, leading to recurrence.
New discovery: The regional characteristics of tumor cells
On November 22, 2024, a study titled "Single-cell multi-omics sequencing uncovers region-specific plasticity of glioblastoma for complementary therapeutic targeting" was published in Science Advances by the teams of Chen Liang and Gu Ying from the BGI Research Institute and the team of Liu Baohui from Wuhan University. In this study, single-nucleus RNA sequencing (snRNA-seq) and single-nucleus chromatin accessibility sequencing (snATAC-seq) technologies from the BGI platform were utilized to systematically analyze samples from GBM patients. These technologies enabled the observation of tumor cell gene expression and the capture of their epigenetic characteristics, thereby providing a novel perspective for revealing the regional characteristics of tumors. The data have been uploaded to the CNGB website (https://db.cngb.org/cnsa/ ; CNP0003766) and an online webpage has been constructed to facilitate exploration by researchers (https://db.cngb.org/cdcp/visualization?project=CNP0003766)

Result 1: Characteristics of State Transition
The study revealed that tumor cells in the tumor core region (TC) predominantly exhibit an astrocyte-like (AC-like) state, whereas in the peritumoral brain tissue region (PTB), oligodendrocyte precursor-like (OPC-like) cells are more prevalent. These findings suggest that: 1) Tumor cells undergo transformation through environmental adaptation. When invading surrounding tissues, tumor cells may acquire the characteristics of neural precursors through interactions with local healthy cells. 2) Cells in certain states exhibit greater diffusibility. The study further indicates that tumor cells in a high OPC-like state are more likely to spread to surrounding tissues.
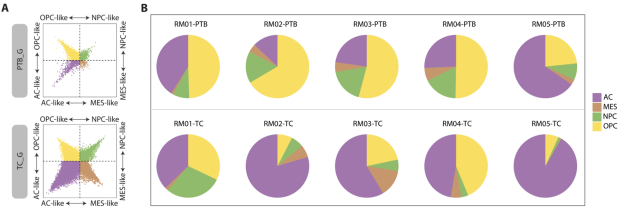
Figure 1 The state of tumor cells changes in the PTB region
Result 2: Regulatory Differences of Key Transcription Factors
Significant differences in molecular regulation between cells in the tumor core region and those in the surrounding region were revealed through further analysis. In the tumor core region, the activity of Activator Protein 1 (AP-1) is relatively high but gradually weakens in the surrounding region. Conversely, the activity of BACH1 is significantly enhanced in the surrounding region. These two transcription factors play crucial roles in tumor invasiveness and state transition. The study indicates that merely inhibiting AP-1 may not be sufficient to completely eliminate the spreading tumor cells, while the increased activity of BACH1 suggests new potential therapeutic targets.
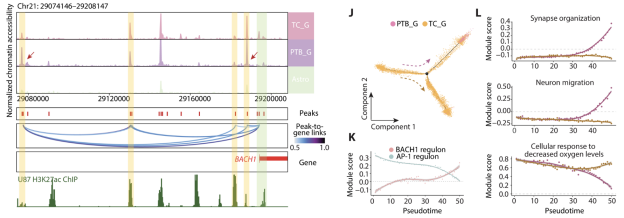
Figure 2 The transcriptional regulation of tumor cells changes after invasion
Result 3: The Potential of Combination Therapy
To verify the potential of these transcription factors in the treatment of GBM, a series of functional experiments were designed by the research team to explore the therapeutic effect of jointly targeting AP-1 and BACH1. This strategy has demonstrated significant curative effects in mouse models.
Figure 3 Combined treatment significantly improves the curative effect
New Direction: Treatment Based on Regional Characteristics
This study proposes a novel approach for the treatment of GBM. By deeply analyzing the regional heterogeneity of tumor cells, the study not only reveals the molecular regulatory mechanisms of tumors but also provides a solid theoretical foundation for future combination therapies targeting dual targets.
If GBM is likened to a battle of attack and defense, then understanding the "transformation technique" and the "lurking technique" is key to addressing its recurrence. This precision treatment strategy, based on regional characteristics, may herald a new chapter in cancer research.
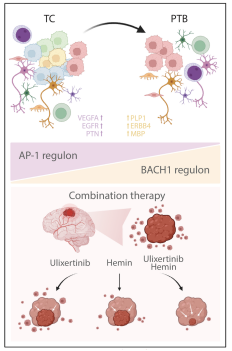
Figure 4 A new treatment strategy targeting the heterogeneity and invasiveness of glioblastoma
Reference News:
https://www.science.org/doi/10.1126/sciadv.adn4306